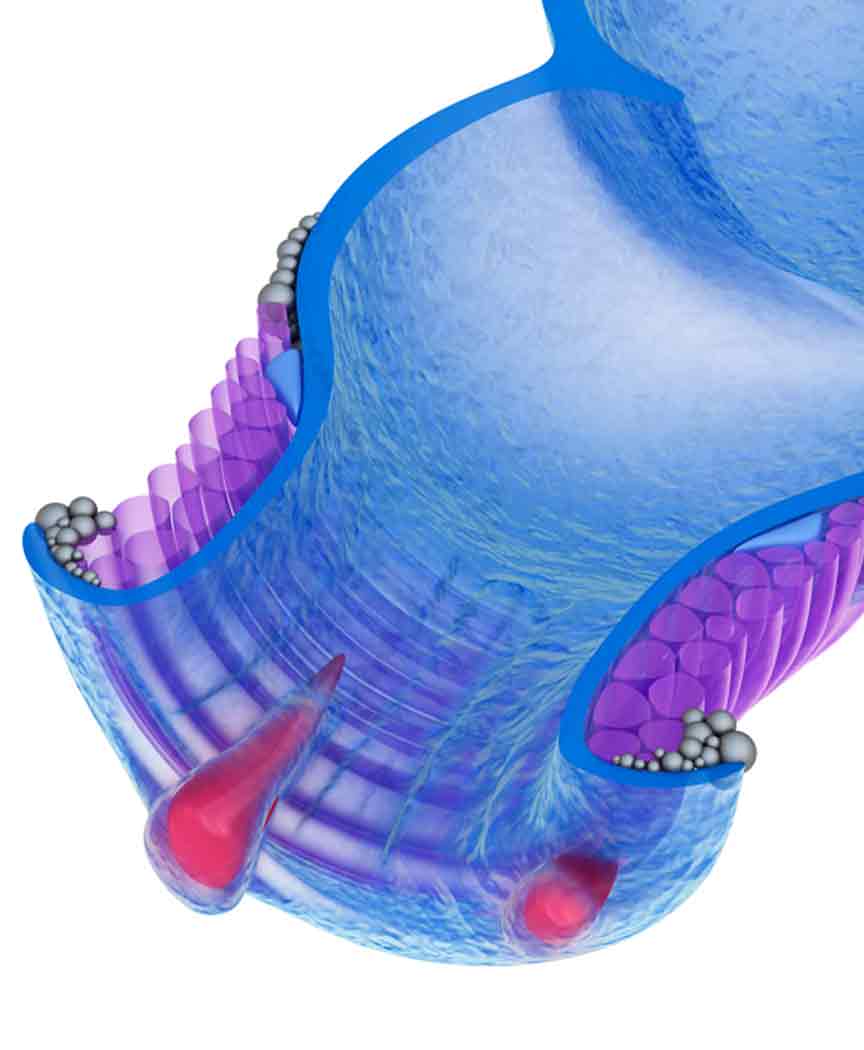
THD is a minimally invasive procedure meant to treat internal hemorrhoids.
Oftentimes, hemorrhoids are treatable with topical creams, home care methods that may include sitz baths, efforts to minimize constipation such as upping your fiber intake, or minimally invasive procedures like injections or coagulation techniques.
Another option a gastrointestinal tract (GI) specialist may recommend is a procedure referred to as transanal hemorrhoidal dearterialization (THD). It’s normally a treatment for patients with grade 2, 3, or 4 hemorrhoids.
What is THD Treatment?
Also referred to as hemorrhoid ligation, transanal hemorrhoidal dearterialization is a treatment that involves the use of a special hollow lighted tube called a proctoscope and a Doppler ultrasound probe. Hemorrhoid banding or rubber band ligation is a similar procedure.


How is it Performed?
THD may be performed with conscious sedation, a numbing agent, or local or general anesthesia. The Doppler probe is used to locate the hemorrhoidal arteries that are affected by the swollen tissues. After the correct terminating branch of the affected artery is found, it is tied off with an absorbable suture.
Since the procedure is carried out in an area without sensory nerves (above the dentate line), the sutures won’t be felt. There is also no need to remove excess tissue. Instead, the repair lifts the affected tissue back to its correct position. The goal with THD treatment is to achieve a firmer attachment to the deeper layers of the rectal wall.
Candidates for THD Treatment
Ideal candidates for the THD procedure are individuals with internal hemorrhoids not responding well to other treatments. It’s generally not recommended for individuals with bleeding issues or serious infections in the affected area. Prior to the procedure, patients are typically advised to stop taking blood thinners or other medications that may cause bleeding problems.
Benefits for Patients
Because fine instruments are used, there is little or no disruption to nearby tissues and structures. This typically means there’s very little discomfort during and after the procedure. Hemorrhoidal tissue does not need to be cut or removed with THD treatment, which further reduces post-operative complications – especially when compared to what may be experienced with hemorrhoid removal. Also, the blood-supplying arteries are sutured and not just tied off, like what happens with rubber band ligation. This added step means there is little risk of the affected tissue coming loose or irritated. Additional benefits associated with THD treatment include:
- Reduced risk of excessive bleeding during the procedure
- Low recurrence rates
- Better long-term results
THD treatment is considered a safer and gentler alternative to traditional hemorrhoid surgery, which usually involves either complete removal of excess tissue (hemorrhoidectomy) or stapling (stapled hemorrhoidectomy). However, there may be instances when stapling is performed at the same time THD treatment is done, especially if the hemorrhoid has prolapsed (fallen down from the rectum so that it’s visible through the anus). Risks associated with the THD procedure are minimal. There may be some temporary discomfort in the rectal area, but otherwise you should be able to resume your normal activities within a day or two.