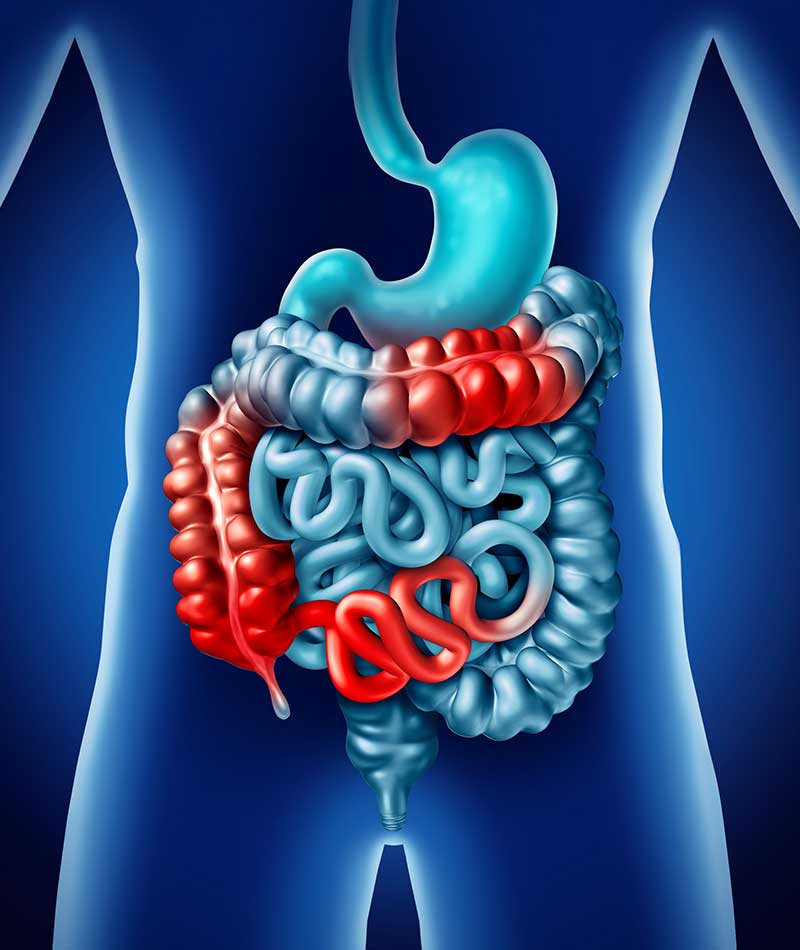
Abdominal pain and bloating are just some of the uncomfortable symptoms associated with irritable bowel syndrome (IBS), a chronic gastrointestinal disorder that affects the colon (large intestine).
Contrary to what some people may believe, IBS does not increase the risk of developing colorectal cancer. And while it can be an uncomfortable condition, most people do respond well to diet adjustments and other conservative treatments often recommended by a GI doctor.
Irritable Bowel Syndrome Causes and Symptoms
Affecting women more often than men, IBS sometimes develops because of weak intestinal contractions, which are necessary to move food along through your digestive tract. Nerve-related issues and intestinal inflammation may also contribute to IBS. In some instances, diarrhea caused by bacteria or a virus and imbalances with bacteria levels within the “gut” can also cause IBS to develop. There’s also some evidence suggesting food allergies may trigger symptoms, although this is rare.
Abdominal pain, cramping, and bloating are IBS symptoms often relieved by making a bowel movement. If you have this condition you may also experience the following symptoms on a regular basis:
- Changes in bowel movements or habits
- Food intolerance that develops suddenly
- Diarrhea or constipation
- Excess gas
- Increased fatigue or difficulty sleeping
- Mucus in stool

How a Diagnosis Is Made
You may be referred to a GI doctor because of IBS if you are experiencing severe symptoms or related issues such as weight loss, rectal bleeding, difficulty swallowing, or abdominal pain that’s not relieved after a bowel movement. There is no specific testing that’s done to diagnose IBS. Instead, efforts are made to rule other conditions that may be causing your symptoms. If one of them is diarrhea, you may be tested for celiac disease (gluten intolerance). In addition to a review of your medical history and a discussion of your symptoms, IBS diagnosis may involve:
- An upper endoscopy
- Stool tests
- A flexible sigmoidoscopy to view part of the colon
- CT scans or X-rays
- A breath test to check for bacterial overgrowth
Possible IBS Treatment Options
If IBS symptoms are mild, you may be advised to make diet and lifestyle changes to manage the condition. Suggestions may include avoiding high-gas foods, certain carbohydrates, or trigger foods, drinking more water and other healthy fluids, exercising regularly, and improving your sleep habits.
Symptoms may also be controllable with Linaclotide (Linzess), Alosetron (Lotronex), and other medications often prescribed for IBS sufferers. If underlying conditions or digestive problems are contributing to IBS issues, a GI doctor might recommend a treatment plan that includes:
- Laxatives or fiber supplements
- Over-the-counter or prescription anti-diarrheal medications
- Selective serotonin reuptake inhibitor (SSRI) antidepressants if depression is contributing to or related to your symptoms
- Pain meds to relieve abdominal discomfort
Because stress is also a possible IBS symptom trigger, you may be able to reduce your risk of developing this condition if you find ways to manage your stress. Some patients achieve this goal with counseling, while others see a reduction in symptoms if they combine traditional IBS treatment with mindful meditation, biofeedback, controlled breathing, and similar relaxation techniques.