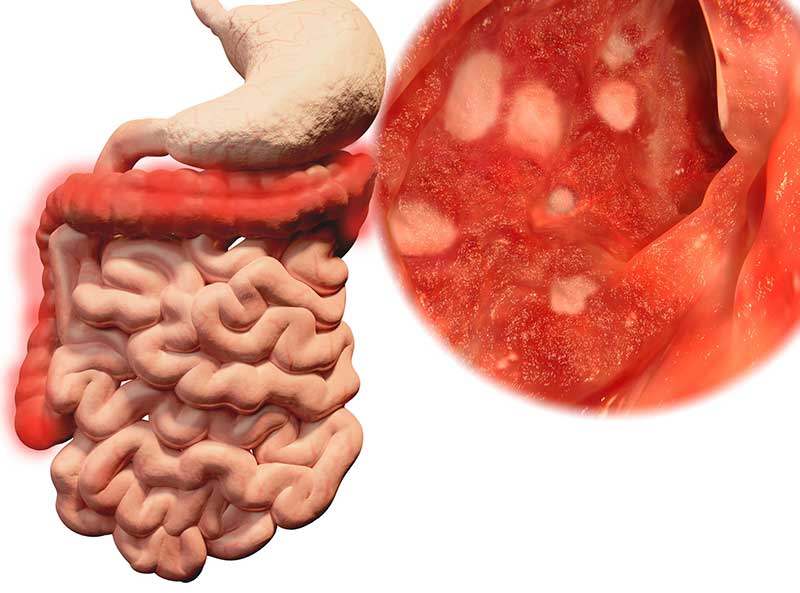
Ulcerative colitis is a condition of the digestive system that can lead to serious complications if left untreated.
With an accurate and timely diagnosis and an appropriate treatment plan, however, it is possible to manage symptoms or to achieve lengthy periods of remission.
What Are the Signs of Ulcerative Colitis?
Patients may experience different symptoms when it comes to this form of inflammatory bowel disease. It is a good idea to note the frequency and severity of the signs in order to describe them during an appointment. Common ones include
- Chronic diarrhea
- Bloody stools
- Abdominal cramping
- An inability to have a bowel movement with or without a feeling of urgency

How Is a Diagnosis Made?
Once symptoms become evident, an appointment with a physician may need to be arranged. In order to diagnose ulcerative colitis, some tests often need to be performed first. A blood test, for instance, can further indicate if ulcerative colitis is possible by diagnosing anemia. A stool sample could also be collected in order to rule out certain types of infection. Some cases require a more invasive examination of the lower digestive tract, however. Under such circumstances, a colonoscopy or a flexible sigmoidoscopy could be performed. Both procedures involve the introduction of a thin flexible tube equipped with a camera or light into the rectum or colon for the purpose of better visualization. The suspicion of a serious complication could prompt the need for imaging tests. The perforation of the colon or severe inflammation could be noted when reviewing such results.
What Treatment Options Are Available?
Some milder symptoms can be managed with anti-inflammatory, pain-relieving, or immunosuppressant medications. Lifestyle choices can also affect flare-ups. Stress or diet could be influential in how often episodes of inflammation occur. Moderate or severe symptoms may warrant a more invasive intervention. These might involve options like:
- An ileal pouch anal anastomosis
- An ileal stoma
- A proctocolectomy
When an ileal pouch anal anastomosis is recommended, the surgeon attaches a pouch to the anus during a restorative proctocolectomy. The pouch, created using a portion of the small intestine, serves as a place to collect waste in a discreet manner. A bowel movement can typically be done in the usual way with this option. In circumstances where this isn’t recommended, patients may benefit from an ileal stoma. A bag, an external ileostomy pouch, is placed over a permanent opening, the ileal stoma, made in the abdomen. The pouch is designed to collect waste.
A traditional proctocolectomy is generally reserved for severe cases, such as when complications become potentially life-threatening, and involves the removal of the rectum and colon. The way each person will manage the removal of waste from the body is determined on the factors involved in each case but will generally warrant an internal or external pouch for collection.
Though flare-ups of ulcerative colitis can vary in frequency and noticeable symptoms, managing them might bring about remission. Bringing any concerns an individual might have regarding persistent and unusual GI symptoms to the attention of a physician is the first step toward taking a proactive measure toward treatment and recovery.